In the world of non-surgical cosmetic enhancements, lip fillers have surged in popularity, offering a quick and effective way to achieve fuller, more defined lips. Among the various products available, Juvederm stands out for its quality and effectiveness. If you are considering enhancing your lips, read on to discover the benefits of Juvederm lip fillers…
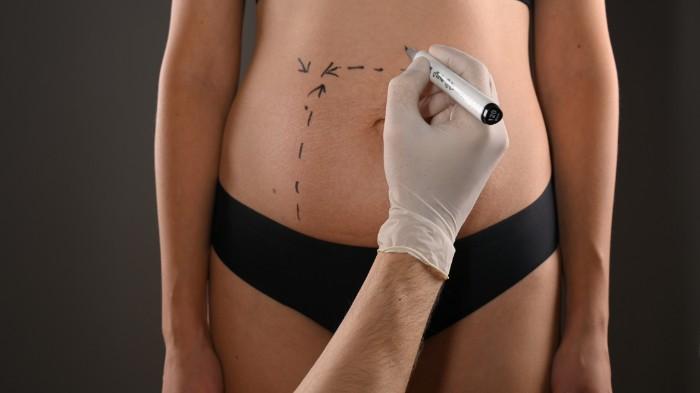
5 Things to Expect During Liposuction Recovery
Liposuction is the second most popular cosmetic surgery treatment, according to the American Society of Plastic Surgeons. It’s a major procedure that removes unwanted fat in certain areas of your body. Your doctor performs this surgery by sculpting and contouring the areas of your body to permanently remove fat cells. However, understanding what to expect…
What is Renuvion?
Renuvion is a minimally invasive procedure that smooths skin for an overall younger and tighter-looking appearance. Other non-invasive treatments that are used to try to tighten skin are limited because they can only treat the outermost layer of skin. Renuvion is different because it delivers a unique combination of radiofrequency and helium plasma energy under…
Plastic Surgery for Men: Common Procedures and Considerations
There’s no doubt that the field of plastic surgery is changing. Once stigmatized as the exclusive domain of women, cosmetic surgery is now just as commonly sought after by men. Whether it’s the quest for an ideal body image or the pressure to maintain a youthful appearance, the male demographic opting for plastic surgery is…
What Is truSculpt Flex And How Does it Work?
The pursuit of a sculpted, lean physique has evolved from being a mere indulgence of the rich and famous to a common desire among fitness enthusiasts, wellness buffs, and those embracing holistic health. Enter truSculpt Flex—a revolutionary body sculpting technology that’s redefining our approach to muscle toning and strength-building, tilting the scales towards a safer,…
A Comprehensive Comparison of Panniculectomy and Abdominoplasty
In many patients, the primary problem is an overabundance of fatty tissue underneath the skin, which can be addressed with weight loss either from dieting, exercising, or in more severe cases weight loss surgery. But when it comes to a substantial weight loss journey, the unsightly presence of the excess skin seems to be quite…
Happy New Years!
This is the time of year when a lot of people make their New Years Resolutions. I think one of the most common resolutions people make is to start working out and getting into shape. Working out can help you lose weight and tone or build up your muscles. But did you know that you…
Why Hydrafacials Are Becoming the Go-To Skincare Treatment for Many Celebrities
Celebrities are always looking for new and innovative ways to take care of their skin, and there’s one treatment that’s become particularly popular in recent years – the Hydrafacial. This facial treatment uses a unique technology to cleanse, exfoliate, and hydrate the skin all in one go, leaving it looking and feeling refreshed and rejuvenated.…
CASE STUDY – GYNECOMASTIA (MAN BOOBS OR MOOBS)
This 25-year-old man had always been self-conscious of his chest. Ever since puberty, he felt that his breasts were too big. He worked out a lot, especially on his pecs, but could not improve the appearance. About 1 out of every 3 guys get enlargement of their breasts/glands at puberty (gynecomastia) due to hormonal changes.…
The Power of Morpheus8 Skin tightening: A Revolutionary Way to Rejuvenate Your Skin
Are you tired of aging skin that just won’t go away? Have you ever heard of Morpheus8? It is a revolutionary way to rejuvenate skin that is fast gaining popularity in the beauty industry. This treatment helps to improve skin complexion and texture for a more radiant and youthful appearance. In this blog post, we’ll…