In recent years, achieving a well-defined jawline has become a significant beauty goal for many. With advancements in cosmetic procedures, non-surgical options like jawline fillers have gained popularity due to their less invasive nature than surgical jawline contouring. At La Belle Vie Plastic Surgery, we use high-quality products like Juvederm to help you achieve the…



Some of the worst words a woman can hear are, “I’m sorry, but the tests came back, and they show that you have breast cancer.”
Typically, when someone is diagnosed with breast cancer, their doctor refers them to a general or oncologic surgeon to undergo a mastectomy. A mastectomy is a major surgery that removes a woman’s breast(s) and tissues where the cancer is out of control.
This procedure seeks to remove all the cancerous cells in the breasts. Once removed, the option of breast reconstruction surgery is suggested in order to reconstruct the shape of the woman’s breasts permanently.
Let’s discuss everything you need to know about breast reconstruction surgery.
What Is Breast Reconstruction Surgery?
Breast reconstruction surgery is performed by a plastic surgeon either at the time of your mastectomy or after you have healed from a mastectomy.
The surgeon helps to recreate your breasts using parts of your body tissue or through artificial means.
Reconstruction: Knowing What to Expect
Several crucial factors influence the timing of your breast reconstruction surgery:
- Risk Assessment: Evaluate potential risks associated with surgery, including weight management and smoking habits.
- Physical Examination: Undergo a comprehensive physical examination to assess your overall health and suitability for the procedure.
- Post-Surgery Treatment Plan: Determine the types and frequency of treatments required after surgery for optimal recovery.
Consult with your healthcare provider to explore the most suitable options tailored to your needs. Don’t hesitate to address all your concerns and inquiries during your discussions.
Deciding If Reconstruction Surgery Is for You
Every woman must make the choice herself. Some women may opt not to have reconstruction surgery, but you will have to determine if you are willing to live the rest of your life without your breasts.
Here are some reasons some women choose to have breast reconstruction surgery:
- Recover self-esteem
- Wanting a balanced chest when wearing her bra and bathing suit
- Allow clothes to have a better fit
- To once more feel whole with reconstructed breast shape
- To have reconstructed areolas and nipples
What Are Your Options?
Women have several options when it comes to choosing how to implement their reconstructive breast surgery. Sometimes more than one operation is needed.
Breast reconstruction surgery is a major surgery, so be prepared to take your time and rest as much as possible.
You don’t want to make uninformed decisions, so make sure you are open and honest with your doctor regarding any questions and concerns you may have.
Here is a list of several options for you and your doctor to discuss:
Flap Procedure
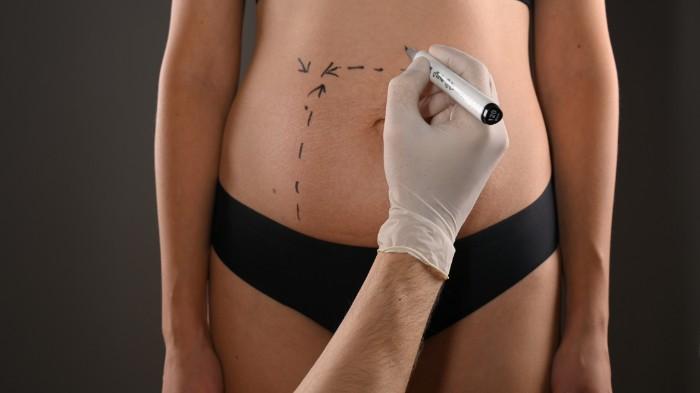
Flap Procedure, in reconstruction, is when the surgeon reconstructs your breasts with tissue from your body. Another name for this procedure is Autologous Tissue Reconstruction.
The places the surgeon takes tissue from for your breast reconstruction include:
- Stomach
- Thighs
- Buttocks
- Back
Let’s look at some positives and negatives of the Tissue Flap Procedure.
Pros:
- Breasts look more natural with this procedure used
- Breasts grow or shrink with weight gain/loss
- Never have to worry about replacing them
Cons:
- Longer recovery time
- More surgery required
- Scar tissues from reconstruction area as well as from where the tissue was taken from
- Possible damage or weakness to muscles
- Possible hernias in the abdomen
- Due to blood vessel issues, this procedure is not recommended for women who have diabetes, vascular disease, smoke, or have connective tissue disorders (i.e., EDS).
Implants
Besides flap procedures, another option is to have a surgeon place a silicone shell filled with a substance to reconstruct the breast’s shape. The filling options for these silicone pieces are:
- Gel—different variations of thickness and gel options such as “cohesive gel” and form stable gel.
- Saline—saltwater that has been sterilized
Implants can be placed at the same time as a mastectomy or can be delayed until after healing. Let’s discuss some of the pros and cons.
Positives:
- Don’t require as much surgery as flap tissue reconstruction
- Boosts self-esteem with shape and size
Negatives:
- Needs to be replaced if they rupture or develop leaks
- Leaks or ruptures can lead to breast cancer, reproductive issues, and connective tissue disorders
- Possibility of rare cancer (Anaplastic Large Cell Lymphoma) associated with textured implants
Areola and Nipple Reconstruction
Most of the time during a mastectomy, the nipples must also be removed. When you decide to have reconstruction done, there are several options for restoring your areolas and nipples.
This surgery is considered less major and can be an outpatient surgery (not admitted to the hospital). This will usually take place about 4 months after breast reconstruction. Here are several restoration options:
- Reconstruction using tissue from the new breast
- 3-dimensional tattoo of nipple and areola
- Prosthetic nipple procedure—where silicone is designed to match the size, texture, and shape of the nipple and can be removed from the breast when you choose.
Whichever way you choose to go, remember that only you can make the decision for what you feel is best for your body and mental health.
Breast Cancer Survivor: Living and Coping
It is imperative to your continual health that you have frequent medical follow-ups. Here is a list of follow-up practices you should continue with:
- Doctor Visits: every few months until completely cancer-free; usually at the 5-year mark, you need to be seen once every year
- Pelvic Exams: discuss with your doctor
- Mammograms: 6-12 months after surgery and then annually
- Tests for bone density: discuss with your doctor
- X-Rays and Bone Scans: only if your doctor requests these
Remember that you are a warrior. You have fought something that no human being should have to go through—and you survived. You are tougher than you look or feel and are strong enough to take on the next phase of healing—breast reconstruction surgery!
Final Thoughts
Considering a second opinion from another medical professional before undergoing reconstruction surgery is highly advisable. Prioritize making well-informed decisions before committing to any major surgical procedures.
Additionally, discussing the option of joining a survivor support group with your doctor can provide invaluable emotional support. Online support groups on social media platforms offer a platform to connect with fellow survivors, providing advice, encouragement, and hope, which can significantly contribute to your mental and emotional well-being during this challenging time.
Breast reconstruction surgery not only restores physical appearance but also plays a vital role in rebuilding self-esteem and resuming normal daily life for women post-cancer. It symbolizes the journey of putting the pieces of life back together after a challenging battle against cancer.
For further information and to schedule your consultation, feel free to reach out to us today. We’re here to assist you every step of the way.